Acknowledgement
This guidance uses the terms ‘woman’ and ‘mother,’ which are intended to be inclusive of anyone who may use other self-identifying terms and aims to encompass all for whom this guidance is relevant.
Consumer Engagement Statement
All interactions between health care staff with consumers (women, mothers, patients, carers and families) should be undertaken with respect, dignity, empathy, honesty and compassion.
Health care staff should actively seek and support consumer participation and collaboration to empower them as equal partners in their care.
Definitions/Abbreviations
Nausea and vomiting in pregnancy is defined as symptoms of nausea, vomiting and/or dry retching commencing in the first trimester without another cause.1
| Abbreviation | Description |
| 5-HT | 5-hydroxytryptamine |
| BD | Twice daily |
| EDS | Edinburgh Depression Score |
| H. Pylori | Heliobacter Pylori |
| H2 | Histamine type 2 receptor antagonists |
| HG | Hyperemesis Gravidarum |
| HITH | Hospital in the Home |
| IgM | Immunoglobulin M |
| IV | Intravenous |
| MSU | Mid-stream urine |
| NVP | Nausea and Vomiting in Pregnancy |
| OD | Once daily |
| PPI | Proton Pump Inhibitors |
| PUQE | Pregnancy-Unique Quantification of Emesis and Nausea |
| QID | Four times daily |
| T 3 and T4 | Triiodothyronine (T3) and thyroxine (T4) |
| TFT | Thyroid Function Test |
| WCC | White Cell Count |
Nausea and vomiting during pregnancy can have a profound effect on a woman’s health and quality of life. Therefore, it is important to recognise and manage these conditions early.1
For most women, the condition is self-limiting, with symptoms resolving by 20 weeks gestation, but prolonged symptoms can be debilitating and distressing.
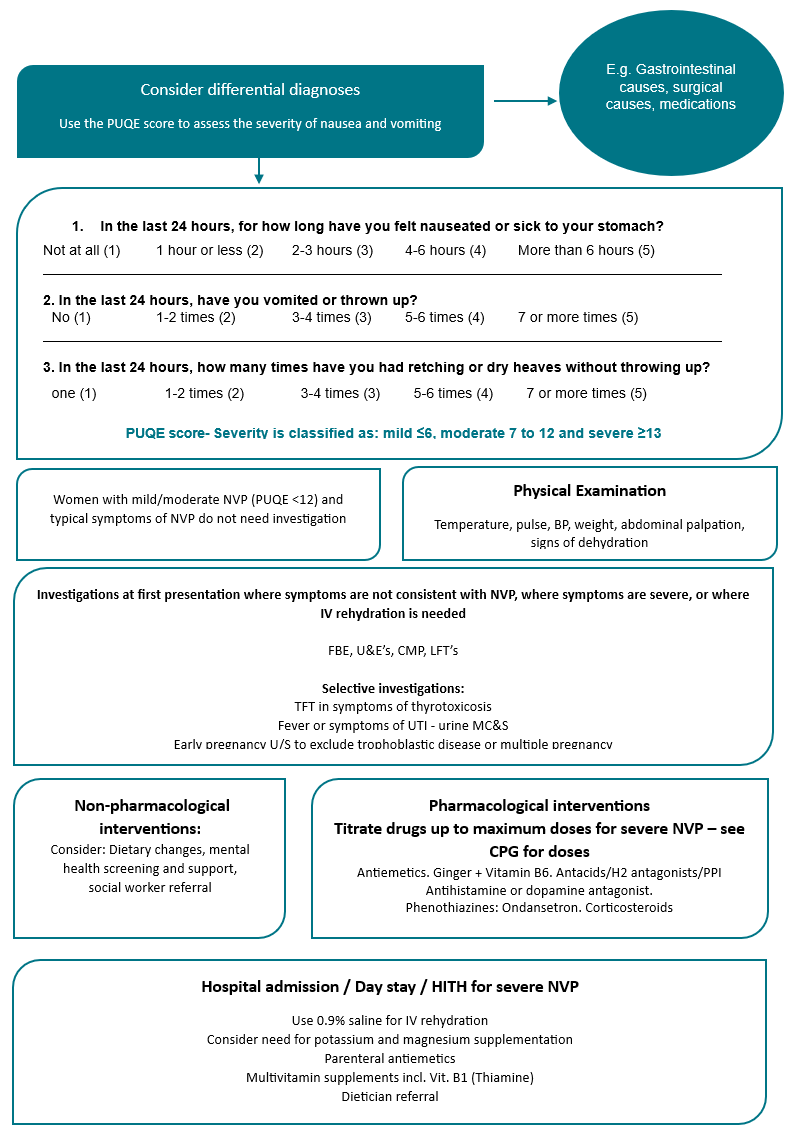
Assessment
Women should be asked about NVP at visits between 4 -16 weeks gestation.
History should include:
- Frequency and duration of symptoms
- Symptoms suggestive of other diagnoses (See ‘differential diagnoses of NVP’)
- Presence of haematemesis - The vomitus of NVP is usually non-bilious and non-bloody, although haematemesis may occur in the context of Mallory-Weiss tears.
For women reporting substantial symptoms, severity should be assessed using an assessment tool. One validated assessment tool is the Motherisk Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) scoring index.2
The PUQE score assesses the severity of nausea and vomiting with three questions relating to the duration of nausea and frequency of vomiting and dry retching symptoms.
The addition of a fourth question to the PUQE-24 score:
“On a scale of 0-10, how would you rate your wellbeing? 0 (worst possible) 10 (the best you felt before pregnancy)”
has been shown to correlate with hydration status but is not routinely included in severity scoring.
| ||||
| Not at all (1) | 1 houror less (2) | 2-3 hours(3) | 4-6 hours(4) | More than 6 hours(5) |
| 2. In the last24 hours, haveyou vomited or thrown up? | ||||
| No (1) | 1-2 times(2) | 3-4 times(3) | 5-6 times(4) | 7 or more times(5) |
| 3. In the last 24 hours,how many timeshave you had retching or dry heaveswithout throwing up? | ||||
| None (1) | 1-2 times(2) | 3-4 times(3) | 5-6 times(4) | 7 or more times(5) |
Severity is classified as: mild ≤6, moderate 7 to 12, and severe ≥13.
The inability to eat and drink, significant weight loss and/or significant limitation of activity, irrespective of the PUQE-24 should also be considered as a measure of severity.
Hyperemesis Gravidarum
Hyperemesis Gravidarum is a more severe subset of NVP, defined as all the following3
- Symptoms starting <16 weeks gestation
- Severe nausea and/or vomiting (PUQE-24 ≥ 13)
- Inability to eat and/or drink normally
- Strongly limiting daily activities
Any validated scoring system can be used to guide initial treatment, but subsequent management decisions should be based on the response to treatment following the principles of management discussed below.
Differential Diagnosis of NVP
(more common causes are in bold)
GastrointestinalInfectious gastroenteritis Gastro-oesophageal reflux disease-Helicobacter Pylori Infectious hepatitis Pancreatitis Biliary tract disease Peptic ulcer disease Bowel obstruction Gastroparesis Appendicitis Peritonitis |
GenitourinaryUrinary tract infection including pyelonephritis Ovarian Torsion Nephrolithiasis |
Central-nervous system diseaseMigraine Infection Tumours Raised intracranial pressure Vestibular system pathology: labyrinthitis, Meniere’s disease |
Metabolic/ToxicDrugs-including pregnancy vitamins Use and/or withdrawal of cannabinoids or other illicit drugs Diabetic ketoacidosis Addison’s disease Thyrotoxicosis Non-infectious hepatitis Hypercalcemia Eating Disorders |
Physical examination
- Temperature, BP, pulse
- Weight, including assessment of percentage weight loss
- Palpation of the abdomen for abdominal tenderness and signs of peritonism
- If the history is suggestive of a central nervous system cause:
- An assessment for neck stiffness and signs of raised intracranial pressure
- Signs to support a diagnosis of dehydration include decreased skin turgor, dry mucous membranes, decreased urine output, concentrated urine and postural drop in blood pressure.
Investigations
Women with mild-moderate nausea and vomiting of pregnancy (PUQE-24 ≤12), where symptoms are not suspicious for HG or another diagnosis, do not need investigation.
Consider investigations if symptoms are severe or where symptoms are not consistent with NVP
Blood tests:
- urea/electrolytes/creatinine
- liver function tests
- calcium/magnesium/phosphate
- Early pregnancy ultrasound to diagnose gestational trophoblastic disease or multiple pregnancy, unless already done
Selective based on symptoms
- TFTs in women with symptoms of thyrotoxicosis
- fever or symptoms of UTI – MSU, WCC
- in women with refractory HG, consider investigation for H. Pylori with faecal antigen testing or serology for IgM.
Management
- The primary goal of treatment is symptomatic relief without adverse fetal or neonatal outcomes.
Discus target of:
- The ability to eat and drink adequately without necessarily complete resolution of NVP.
- Provide women and their families with information on the risks and benefits of proposed treatment options.
- Psychosocial support.
- Perform routine mental health screening, using the method used in your site, or the Edinburgh Depression Score (EDS). 4
- Repeated screening as indicated, particularly if symptoms are severe and prolonged.
- Consider social work review and psychological support.
Non-pharmacological interventions
- Diet
- Eating small amounts of fluid and food throughout the day, may be helpful
- Referral to a dietician may be appropriate.
- Weak evidence supports the use of acupuncture.
- Some women may choose to use other techniques including herbal remedies, relaxation techniques, hypnotherapy, psychological interventions, emotional support or behavioural interventions/modifications however, these are not supported by published data.
- Discuss with women the potential for harm when using non-prescribed medications, particularly those containing unknown ingredients.
Pharmacological interventions
- Discontinue prenatal multivitamins if they are contributing to NVP:
- the micronutrients to be continued if possible are iodine (150 mcg per day) and folate (at least 400 mcg per day until 12 weeks)
- The timing of administration of pharmacological therapy should reflect the woman’s symptom pattern:
- symptoms often fluctuate during the day and night and therapy should reflect these individual differences.
The choice of antiemetic should be individualised, based on the woman’s symptoms, previous response to treatment and potential maternal or fetal adverse effects:
if an antiemetic is ineffective at maximal dose, discontinue before commencing an alternate agent.
if an antiemetic is partially effective, optimise dosage and timing and only add additional agents after maximal doses of the first agent have been trialled.
Oral therapy is usually commenced first, and parenteral or subcutaneous treatment reserved for more severe cases.
- Written instructions should be provided regarding titrating therapy (up and down) as symptoms change.
- Regular review of therapy is required:
- the natural history of NVP and HG is of spontaneous resolution at some gestations.
- Treatment of NVP and HG may require a range of agents including:
- antiemetics:
- acid suppression
- steroids
- other: e.g. Laxatives, supplements, antidepressants
Commencement and titration of pharmacological treatment for NVP or HG:
Mild-moderate NVP:
- start with ginger ± B6
- add oral antihistamine or dopamine antagonist (Table 1.3) if needed.
- manage/prevent constipation with laxatives
- acid suppression therapy. (Table 1.1)
Moderate-severe NVP or inadequate response to initial treatment:
As above for mild-moderate:
- if effective - continue and titrate to maximal dose
- if ineffective - cease.
Further treatment:
- antihistamine or dopamine antagonist IV/IM until able to tolerate oral (Table 1.3)
- excessive sedation or inadequate response: add /substitute oral or IV ondansetron at least during daytime
Refractory NVP or HG:
As for moderate-severe
- consider addition of corticosteroids (Table 1.6)
- intensify acid suppression
- consider addition of thiamine to prevent Wernicke’s encephalopathy. 5
Table 1. Medications to treat hyperemesis
| Drug | Dosage and administration | Side Effects |
|---|---|---|
| ||
Antacids containing magnesium, calcium or aluminium Mylanta®, Gaviscon®, Gastrogel® | As per product recommendations | Use as a regular, rather than prn medication |
| H2 antagonists | Famotidine 20 mg OD or BD | |
| Proton-pump inhibitors (PPI) | Omeprazole or Rabeprazole 20 mg daily or BD, | Use as a regular, rather than prn medication |
| Pantoprazole or Esomeprazole 40 mg daily or BD | ||
| Lansoprazole 30g daily or bd | ||
| ||
| Ginger | Use standardised products rather than foods e.g. 250 mg TDS-QID [1000mg] | |
| Pyridoxine | 10 to 25 mg PO 3-4x/day [200 mg] Or 37.5 mg combined with ginger 600 mg up to 2x/day | |
| ||
| Doxylamine (Restavit®) | Add 25 mg orally, at night. Increase as tolerated to 12.5 mg in the morning | |
| Metoclopramide (Maxolon®, Pramin®) | 10mg orally threetimes a day for up to 5 days 10mg IV/IM every 8 hours when required for a | Less sedation. To reduce the risk of extrapyramidal side effects- use for the shortest possible duration and lowest effective dose |
| ||
| Prochlorperazine (Stemetil®) | 5 to 10mg orallytwo to threetimes a day 12.5mg IM/slow IV every 8 hours
| Sedation, akathisia, anticholinergic effects, hypotension Rare: dystonia’s, tardive dyskinesia with chronic use Best reserved for evening dosing |
| Promethazine (Phenergan®) | Add another sedating antihistamine: 10 to 25mg orally three to four times a day 12.5 to 25mg IM 4 to 6 hourly | Sedation Best reserved for evening dosing. |
Chlorpromazine
| 10 to 25mg IV/IM every 4 to 6 hours | |
| ||
| Ondansetron (Zofran®) | 4mg to 8mg orally (tablet or wafer) two or three times a day. 4mg IV/IM every 8 to 12 hours
| No sedation Expensive Ensure concurrent management of constipation. Recommended as second line agents |
| ||
Prednisone
May be commenced as hydrocortisone | 40-50 mg/day. | Consider withholding until after 10 weeks' gestation if alternate therapy an option Restrict to refractory cases Wean to 10 to 12.5 mg/day over 7 to 10 days then by 2.5 mg/day every 3 days to minimum effective dose. Increase folate to 5 mg, oral, once per day if prescribing steroids in first trimester |
| 100 mg IV BD [200mg] | ||
| Laxatives and stool softeners | ||
| Use local preference | ||
Inpatient management
- Initial inpatient care is usually required for women with:
- Severe electrolyte disturbance e.g. potassium < 3.0mmol/L
- Significant renal impairment or acute kidney injury: creatinine > 90 mmol/L
- Concurrent significant co-morbidity e.g. Type 1 diabetes, poorly controlled epilepsy, transplant recipients, or others requiring essential medications
- Malnutrition/continuing significant weight loss despite therapy or starvation ketoacidosis
- Associated conditions requiring inpatient management e.g. infection, hematemesis, refeeding syndrome.
Ambulatory Day Stay facilities and/or Hospital In The Home (HITH) services should be utilised for women who require parenteral fluid resuscitation and parenteral anti-emetic administration.
| Ongoing IV rehydration may be needed two to three times a week. IV rehydration | Use Sodium chloride 0.9% Glucose solution should not be used Usually, two or more litres of sodium chloride 0.9% is administered over 2-3 hours If more fluid is needed, reassess hydration status Check electrolytes daily if requiring ongoing IV fluid Consider the degree of dehydration and electrolyte disturbance Add potassium and magnesium if required after checking electrolytes Provide multivitamin supplementation. |
| Parenteral antiemetics |
|
| Thiamine (Vit B1) | Thiamine 100 mg orally or IV daily. |
| Dietitian referral | On diagnosis of HG where first- and second-line treatments do not appear to be effective Where weight loss exceeds 5 per cent of total body weight. |
| Enteral nutrition support |
|
Management of abnormal TFT
Elevated T4 and low TSH are common in early pregnancy and in women with NVP.
- Gestational hyperthyroxinemia (GHT), gestational transient thyrotoxicosis or gestational hyperthyroidism is a transient biochemical thyrotoxicosis, which develops in early pregnancy and resolves before 20 weeks gestation
- Women do not have overt signs of hyperthyroidism and have negative thyroid receptor antibodies
- GHT occurs in approximately 1-3% of women in early pregnancy because placental human chorionic gonadotropin (hCG) is structurally similar to Thyroid Stimulating Hormone (TSH) and can directly stimulate the TSH receptor, increasing thyroid hormone production and suppressing serum TSH
- Do not measure TFTs in women with nausea and vomiting of pregnancy and no diagnostic criteria for HG
- Measure TSH in women with HG or NVP refractory to treatment, or in women with signs and/or symptoms of thyrotoxicosis
- If TSH is below the normal gestational corrected reference range, further testing is indicated:
- repeat TSH, free T4, free T3 Thyroid antibodies including thyroid peroxidase and thyroid receptor antibodies
- thyroid ultrasound if there is goitre, particularly with nodularity.
Management of women who have Gestational hyperthroxinaemia is supportive with appropriate treatment of NVP; anti thyroid medications are not required. Specialist referral is not required.
If an alternative cause for hyperthyroidism is suspected/confirmed, refer the woman to the appropriate specialists e.g. physician or endocrinologist, as well as an obstetrician for ongoing assessment and management of thyroid disease.
Appropriate management of associated NVP should continue.
Further information
Audit and performance improvement
All maternity services should have processes in place for:
- Auditing clinical practice and outcomes
- Providing feedback to clinicians on audit results
- Addressing risks, if identified
- Implementing change, if indicated.
References
- Lowe SA, Bowyer L, Beech A, Tanner H, Armstrong G, Marnoch C, Grzeskowiak L. Position Statement on the Management of Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum [Internet]. SOMANZ; 2023 [cited 2024 Mar]. Available from: https://www.somanz.org/content/uploads/2023/12/SOMANZ-Management-of-NVP-Position-Statement-Updated-Oct-2023-FINAL-1.pdf
- Koren G, Boskovic R, Hard M, Maltepe C, Navioz Y, Einarson A. Motherisk—PUQE (pregnancy-unique quantification of emesis and nausea) scoring system for nausea and vomiting of pregnancy. Am J Obstet Gynecol. 2002;186(5 Suppl 2) doi: 10.1067/mob.2002.123054.
- Jansen LAW, Koot MH, van’t Hooft J et al. The Windsor definition for hyperemesis gravidarum: A multistakeholder international consensus definition. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2021;266:15-22.
- Matthey S, Barnett B, White T. The Edinburgh Postnatal Depression Scale. Br J Psychiatry. 2003 Apr;182:368. doi: 10.1192/bjp.182.4.368. PMID: 12668422.
- Oudman E, Wijnia JW, Oey M, van Dam M, Painter RC, Postma A. Wernicke's encephalopathy in hyperemesis gravidarum: A systematic review. Eur J Obstet Gynecol Reprod Biol. 2019 May;236:84-93. doi: 10.1016/j.ejogrb.2019.03.006.)
Acknowledgments
- Mercy Hospital for Women Nausea and Vomiting in Pregnancy Clinical Guideline.
- The Royal Women’s Hospital. Nausea and Vomiting in Pregnancy – Guideline [Internet]. 2022 [cited 2024, March]. Available from: https://www.thewomens.org.au/health-professionals/clinical-resources/clinical-guidelines-gps/
- Western Health (2022) Nausea and Vomiting in Pregnancy (including Hyperemesis Gravidarum)
- Monash Health Guidelines and Procedures. Pregnancy induced vomiting and Hyperemesis. [Internet]. 2021 [cited 2024, March]. Available from: https://monashwomens.org/health-professionals/clinical-guidelines-and-procedures/#pregnancy
Citation
To cite this document use: Safer Care Victoria. Nausea and Vomiting in Pregnancy Guideline [Internet]. Victoria: Maternity eHandbook; 2024 [cited xxx] Available from: https://www.safercare.vic.gov.au/clinical-guidance/maternity
Outpatient management flowchart
Download
Get in touch
Version history
First published:
February 2018
Reviewed:
October 2024