This is a guideline specifically for the management of tachyarrhythmias in neonates. Advanced Paediatric Life Support (APLS) guidelines are also commonly in use and have minor differences. Use of the guideline that treating clinicians have most familiarity with, is acceptable.
Acknowledgement
This guidance may use the terms ‘woman’ and ‘mother,’ which are intended to be inclusive of anyone who may use other self-identifying terms and aims to encompass all for whom this guidance is relevant.
Consumer Engagement Statement
All interactions between health care staff with consumers (women, mothers, patients, carers and families) should be undertaken with respect, dignity, empathy, honesty and compassion.
Health care staff should actively seek and support consumer participation and collaboration to empower them as equal partners in their care.
Initial steps
Support in the diagnosis and management of neonates with suspected tachyarrhythmia can be obtained initially by contacting PIPER on 1300 137 650 and the RCH Cardiologist can be added to the referral call.
It is helpful to have a 12 lead ECG to send electronically at this time but should not delay the referral call if urgent resuscitation guidance is required.
Cardiology consultation regarding diagnostic and therapeutic management issues is also available at any time through the switchboard of either Monash Medical Centre on (61 3) 9594 6666 or the Royal Children’s Hospital on (61 3) 9345 5522.
Obtain a 12 lead ECG if not already done.
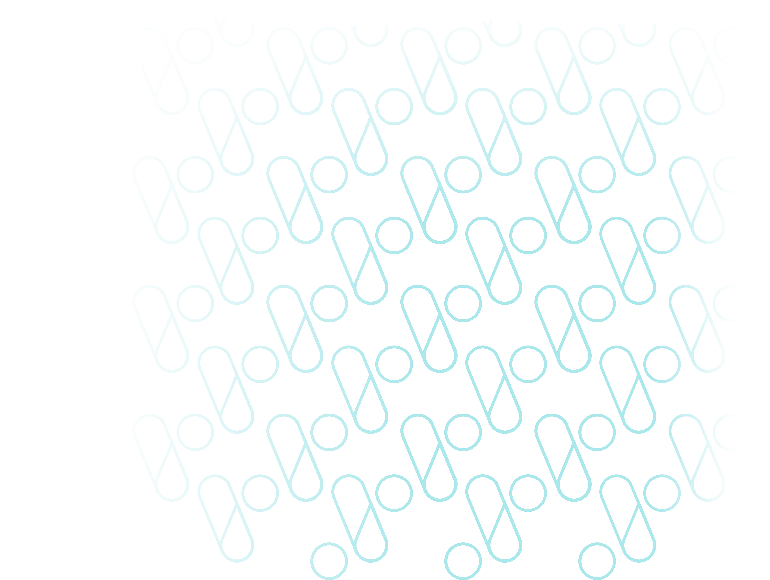
Correct placement of ECG leads
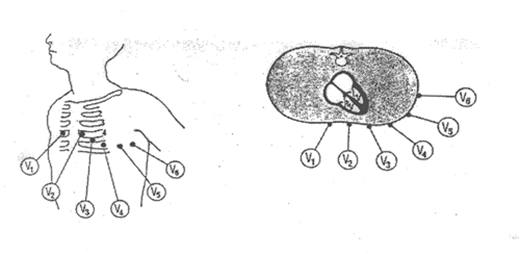
ECG interpretation
| Normal rate P wave: rate, rhythm, axis (P upright in I, aVF) P-QRS relationship: 1:1 association, PR interval < 0.2sec QRS complex: rate, axis, broad or narrow. Normal 0.02–0.08 sec QTc = QT/√RR > 0.46 sec |
Continuous ECG monitoring is preferable (with printing facility if available).
Obtain blood to check blood gas – lactate, glucose, electrolytes including ionised calcium. Consider also collecting blood for full blood examination and thyroid function tests if able.
Stabilisation
Resuscitation takes priority over managing an arrhythmia. 2
Assess patient for cardiopulmonary compromise or signs of heart failure, these include poor feeding, tachypnoea, pallor, delayed capillary refill, sweating, lethargy and irritability.
Obtain IV/IO access and give oxygen if saturations are below 92%.
Differential diagnosis
Sinus tachycardia
Usually up to 220bpm, p wave for every QRS. P wave upright in lead II, III and aVF.
Should vary with stimulation or temperature.
Usually associated with sepsis, fever, pain, hypovolaemia or anaemia.
Investigation and treatment are aimed at managing the underlying cause.
Supraventricular tachycardia
Most common spontaneous-onset arrhythmia in infancy.
Usually > 240 bpm and up to 300 bpm, narrow QRS complex, p waves may or may not be present, not upright in lead II, III and aVF.
Abrupt onset of tachycardia.
The most common mechanism of SVT in neonates is a re-entry atrioventricular SVT (AVRT) with the existence of an accessory pathway to allow retrograde transmission of the atrial contraction in addition to its usual transmission via the bundle of His. 1
SVT management
Vagal manoeuvres
In haemodynamically stable patients, vagal stimulation should be attempted initially.
ECG monitoring should continue throughout these attempts.
This can be achieved by applying a plastic bag filled with ice and water to the face for 10 seconds. Inducing a gag by oropharyngeal suctioning or with a spatula may also be attempted if the resources to do so are more immediately available.
Do not apply pressure to the eyeballs as this can result in retinal detachment.
Adenosine
Is the preferred first-line medication for treatment of neonates with SVT with a palpable pulse. 2,3,4
It has a very short half-life and must be given rapidly via a cannula in a large bore vein or via an IO followed by a rapid flush of 5mL 0.9% normal saline. The antecubital vein is the preferred site with a 3-way tap attached to for administration of adenosine via one port and flush via the other.
- Initial dose: 100 mcg/kg
- Increase in increments of 100 mcg/kg every 2–3 minutes to a maximum of 300 mcg/kg until cardioversion is achieved (a short period of cardioversion with re-starting of the SVT is also a cardioversion and increase in dose is not helpful in this case).
- If patient remains in SVT seek further cardiology/PIPER advice following which doses of up to 500mcg/kg may be given.
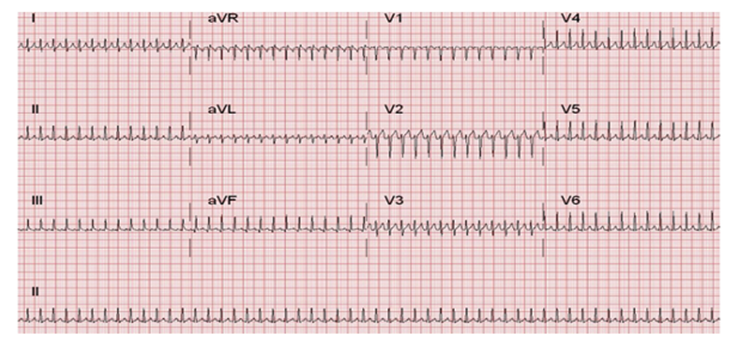
Adenosine administration should always be done with ECG capture on paper or an electronic recording system.
Adenosine works by temporarily blocking the AV node. A brief pause will be seen on ECG before return of sinus rhythm. If this pause is not seen, and sinus rhythm is not achieved, SVT due to a re-entrant atrioventricular pathway is much less likely to be the cause of the observed tachyarrhythmia.
The only contraindication to adenosine is adenosine-deaminase deficiency, a rare form of severe combined immune deficiency, with a worldwide incidence of 1:200,000 to 1:1000,000.
Synchronised cardioversion
If the patient is profoundly hypotensive or pulseless and/or IV/IO access cannot be obtained rapidly, emergency synchronised cardioversion should be first-line management 2 and performed in consultation with PIPER and Cardiology.
Synchronised cardioversion is also performed electively if the patient remains cardiovascularly stable but reversion to sinus arrythmia has not occurred after maximal dose of adenosine. 2
Other antiarrhythmics
Esmolol may be given for refractory SVT after further Cardiology/PIPER consultation.4 It is given by a slow IV infusion with careful haemodynamic monitoring with an initial loading dose of 100–500mcg/kg over 1–2 minutes; followed by an infusion at 25–100 mcg/kg/min. This can be titrated to response in increments of 25–50 mcg/kg/min allowing at least 5 minutes between dose adjustments to assess for response. Maximum dose is 500–1000 mcg/kg/min.
Verapamil must NEVER be given to neonates due to risk of profound hypotension and death.
Wide complex SVT
Can be caused by an aberrant conduction (bundle branch block) or conduction through a pathway (antidromic AVRT) or ventricular tachycardia (VT).
If pulses and blood pressure are normal, treatment as per SVT can be instituted. 2
If pulses are present but there is hypotension or inadequate systemic circulation, treatment should proceed as per VT with synchronised cardioversion. 2
If pulses are absent, the rhythm should be managed as pulseless VT and managed with continuous CPR and defibrillation at doses of 4 J/kg. 2
Ventricular tachycardia
VT is rare in neonates and when it does occur is often associated with an underlying electrolyte abnormality, congenital heart disease (including after surgical repair), cardiomyopathy or cardiac tumour.
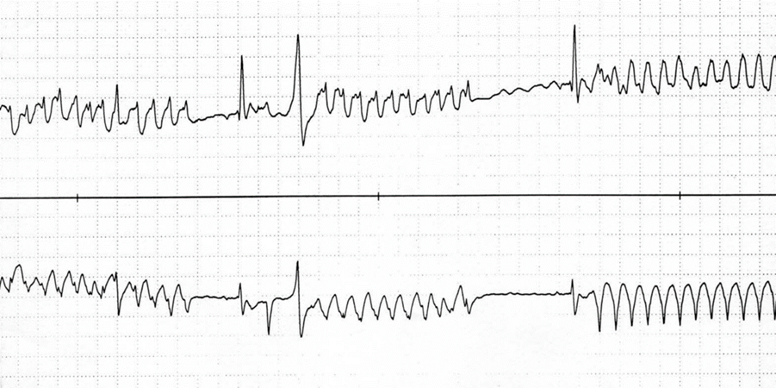
Three or more ventricular complexes without any p-waves and wide QRS complexes with abnormal morphology.
VT management
Synchronised cardioversion is recommended first-line management in a shocked patient. 2
Amiodarone may be recommended following Cardiology consultation, dependent on the history and any identified underlying cause.
Atrial flutter
Can occur in the fetus in the third trimester and in the neonate. Rare later in infancy/childhood. 5
Fetal atrial flutter can cause hydrops. If detected, it may be amenable to maternal beta blockade.
Irregular atrial activity of 280-500bpm with variable conduction (frequently 2:1 AV conduction)
Caused by re-entrant circuits within the right atrium.
Can be associated with structural congenital heart disease.
ECG shows typical ‘sawtooth’ pattern in leads II, III, aVF and V1. This may only become apparent when the AV node is temporarily blocked by adenosine administration.
Treatment is in discussion with PIPER and Cardiology. If there is significant haemodynamic compromise, synchronised cardioversion may be necessary.
Cardioversion
If time and patient stability permits, the patient should be intubated and ventilated and sedated prior to commencement.
Delivery of DC shock must be synchronised with the QRS complex to minimise the risk of converting to another rhythm, including ventricular fibrillation or asystole.
Initial shock of 1 J/kg is recommended, followed by 2 J/kg if necessary.
It is important to be familiar with the defibrillator model and its safe operation in the institution where you work.
Ongoing management
Patients in level 4 or 5 units with access to echocardiography and who cardioverted rapidly with vagal manoeuvres or adenosine may be able to remain there and ongoing management occur in consultation with Cardiology.
All other patients will likely require PIPER retrieval to a centre with Paediatric Cardiology.
Subsequent investigations will include a Holter monitor and echocardiogram as there are four important structural associations of atrioventricular re-entry SVT; all may be silent to clinical examination. These are:
- Ebstein’s anomaly
- congenitally corrected transposition
- dilated and hypertrophic cardiomyopathy
- myocardial tumours.
Follow-up plan
The follow-up plan, including the prescription of maintenance medication, should be made in close consultation with a cardiologist.
- The first-line maintenance medication would likely be a beta-blocker. These should be initiated in hospital for neonates and monitoring for hypoglycaemia should be performed.
- The parents need to be taught how to take the pulse. It may be appropriate for this to be checked prior to putting the baby to sleep and the pulse can be checked if the baby is ‘off colour’.
- Accessory pathway function disappears in 40 per cent of patients by the age of one year. If pathway conduction persists symptoms may settle in the first year only to return at 7 or 8 years of age.
References
- Abbasi E, Vijayshankar SS, Goldman RD. Management of acute supraventricular tachycardia in children. Can Fam Physician. 2023 Dec;69(12) e626-31
- APLS Algorithms
- Australian New Zealand Council on Resuscitation (ANZCOR). Guideline 12.3 – Management of other (non-arrest) arrhythmias in infants and children. Circulation. 2000;102:1291-342.
- Australian Neonatal Medicines Formulary, 2023
- Wojtowicz-Marzec M et al. Successful treatment of neonatal atrial flutter by synchronized cardioversion: case report and literature review. BMC Pediatr. 202;20(1):370.
Citation
To cite this document use: Safer Care Victoria. Tachyarrhythmia in neonates [Internet]. Victoria: Neonatal eHandbook; 2024 [cited xxxx] Available from: https://www.safercare.vic.gov.au/clinical-guidance/neonatal
Downloads
Get in touch
Version history
First published:
August 2013
Reviewed:
October 2024