Acknowledgement
This guidance may use the terms ‘woman’ and ‘mother,’ which are intended to be inclusive of anyone who may use other self-identifying terms and aims to encompass all for whom this guidance is relevant.
Consumer Engagement Statement
All interactions between health care staff with consumers (women, mothers, patients, carers and families) should be undertaken with respect, dignity, empathy, honesty and compassion.
Health care staff should actively seek and support consumer participation and collaboration to empower them as equal partners in their care.
Definitions/Abbreviations
| Blood sugar level (BSL): as measured using a point of care non-glucose oxidase method with a blood glucose meter and reagent strips. These measurements are less accurate at lower levels, therefore a TBG should be performed for any BSL < 2.6 mmol/L. |
| True blood glucose (TBG): as measured by the glucose-oxidase method on a blood gas analyser, in the laboratory or a point of care device e.g. iSTAT measurement. |
| Hypoglycaemia: TBG < 2.6 mmol/L. 1 |
Hypoglycaemia in neonates
Neonatal hypoglycaemia (defined as true blood glucose < 2.6 mmol/L)1 is common, preventable and can both cause and potentiate neonatal brain injury.
This guideline provides evidence-based guidance for identification of newly born infants at risk of hypoglycaemia, clinical signs of hypoglycaemia and management of hypoglycaemia including prevention, screening and treatment in birthing environments, postnatal areas and the neonatal unit. It includes advice about escalation of care and investigations.
Supporting resources
Management flowcharts
To be used in conjunction with this guidance:
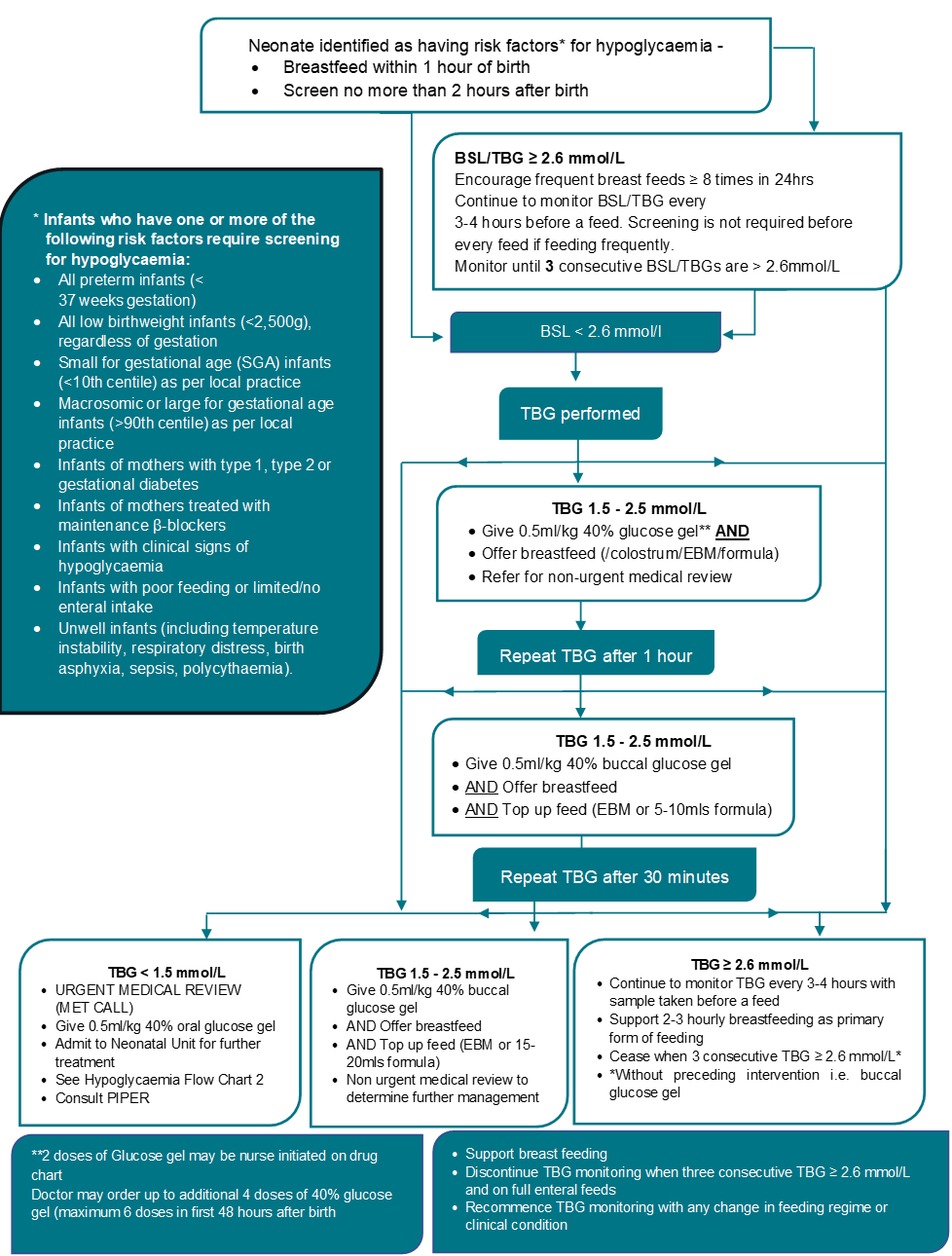
- Flowchart 1 – Management of hypoglycaemia in birthing environments and postnatal wards
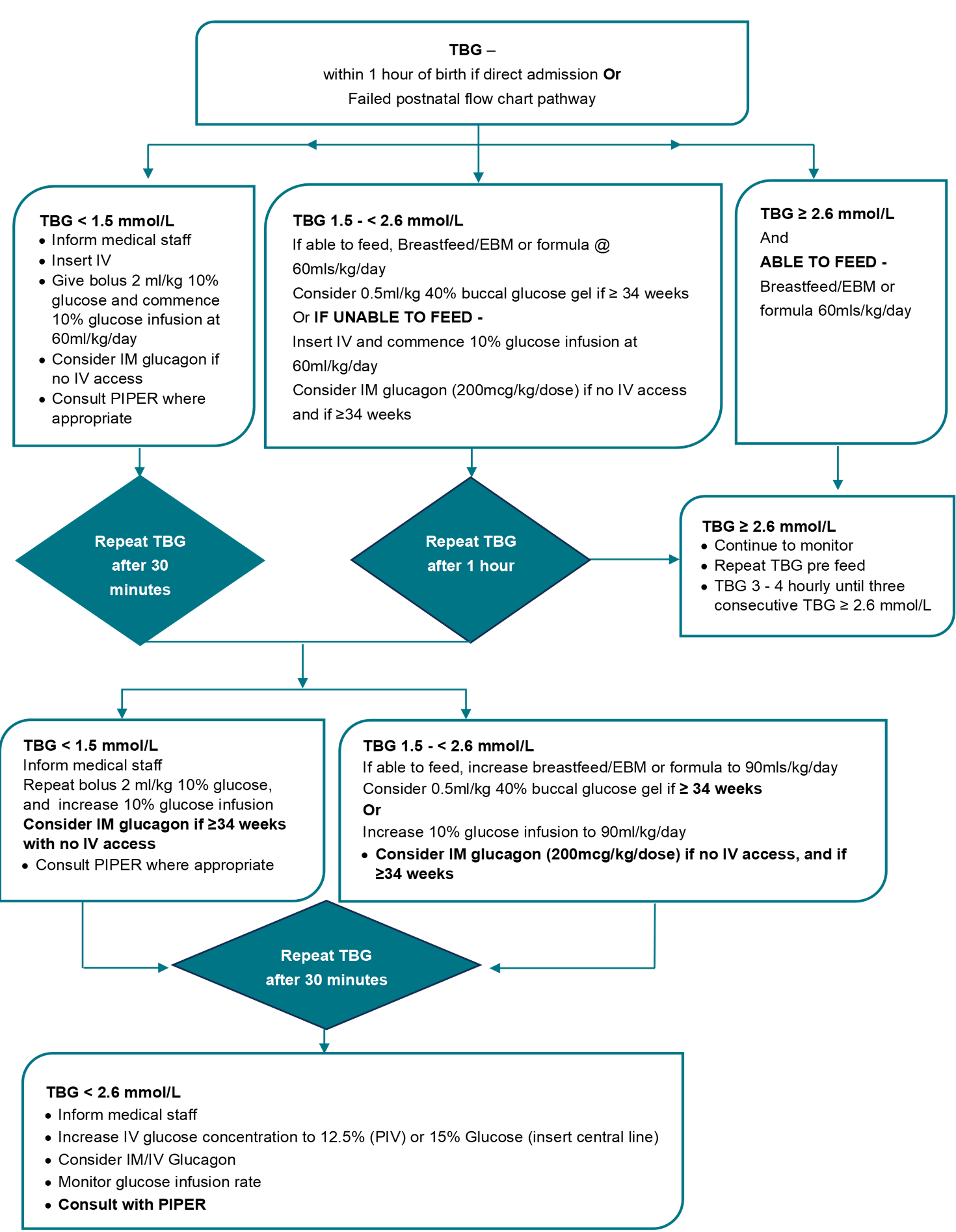
- Flowchart 2 - Management of hypoglycaemia in neonatal units
Parent information
Safer Care Victoria recommends the Queensland Clinical Guidelines Parent Information Hypoglycaemia in newborn babies as a useful resource for parents and caregivers.
Background
Hypoglycaemia is defined as true blood glucose (TBG) < 2.6 mmol/L.1 Although there is ongoing debate regarding the lowest threshold of blood glucose concentration that is considered safe, evidence shows that even single episodes of hypoglycaemia in the neonatal period may be associated with adverse learning outcomes, 2 with a dose-dependent relationship between severe hypoglycaemia and impaired executive function and visual-motor outcomes. 3
In well, term infants, the normal post-partum blood glucose nadir occurs at approximately 90 minutes, with mean minimum blood glucose concentrations of 3.3 mmol/L. 4
The normal post-birth blood glucose nadir occurs earlier with decreasing gestational age. 2 For infants who are admitted to a neonatal unit with multiple risk factors for hypoglycaemia, and those who are in a neonatal unit due to other illnesses, hypoglycaemia may be early and severe.
Currently, intermittent TBG monitoring is the only practical method to screen babies for hypoglycaemia but may miss up to 25% of hypoglycaemic episodes in at risk infants. 5 The use of an enzymatic method to evaluate all blood glucose concentrations reduces the number of false-positive and false-negative results for hypoglycaemia and decreases the number of repeat heel-prick tests required. 6 TBG should be used in preference to a BSL when available, and for ongoing screening in all infants who have had a BSL < 2.6 mmol/L.
Most cases of neonatal hypoglycaemia are transient, related to adaptive metabolic transition from foetal to neonatal life. 7
Assessment
Risk factors
Infants who have one or more of the following risk factors require screening for hypoglycaemia: 8
- all preterm infants (< 37 weeks’ gestation)
- all low birthweight infants, (< 2,500g) regardless of gestation
- small for gestational age (SGA) infants (< 10th centile on growth chart*)
- macrosomic or large for gestational age infants (> 90th centile on growth chart)*
- infants of mothers with type 1, type 2 or gestational diabetes
- infants of mothers treated with maintenance β-blockers
- infants with clinical signs of hypoglycaemia (see below)
- infants with poor feeding or limited/no enteral intake
- unwell infants (including temperature instability, respiratory distress, birth asphyxia, sepsis, polycythaemia).
Note: *Growth chart examples include: WHO Growth Charts 9 (universally adopted in 2012 by all Australian states and territories for infants 0 – 2 years age). Alternatives are Fenton Growth Charts 10and Intergrowth 21 11 In 2020 new Australian birthweight centiles were published in Medical Journal of Australia based on population data collected between 2004 – 2013 by Australian Institute of Health and Welfare National Perinatal Data Unit. 12
History and examination
Clinical signs of hypoglycaemia
Most infants with hypoglycaemia have no clinical signs. 2
Clinical signs that suggest clinically significant hypoglycaemia are non-specific and may include any one or more of the following: 13
- jitteriness
- irritability
- high pitched cry
- cyanotic episodes
- apnoea
- seizures
- lethargy
- hypothermia
- hypotonia
- altered/poor feeding.
Management
Consider sepsis as a cause of hypoglycaemia.
Infants with risk factors for hypoglycaemia
All newly born infants with risk factors for hypoglycaemia should be offered a breastfeed within one hour of birth (if the mother chooses to breastfeed if not formula feed), then at least every 3 hours.
- Infants of mothers who choose to formula feed should be offered the equivalent of 60 mL/kg/day.
- Infants who are unable to feed enterally, for any reason, should have intravenous (IV) access obtained and an IV glucose infusion commenced within one hour of birth.
- Infants with more than 2 risk factors for hypoglycaemia are at increased risk of severe hypoglycaemia 14 and should be referred to a doctor after birth and assessed for potential neonatal unit admission.
Prevention of hypoglycaemia in birthing environments and postnatal wards
Refer to Management of hypoglycaemia in birthing environments and postnatal wards – flow chart 1.
- Dry the infant and encourage early prolonged skin-to-skin contact.
- Keep the mother and infant together if possible
- Maintain temperature between 36.5ºC and 37.5ºC.
Screening
- Assess for risk factors for hypoglycaemia.
- There is no need to measure blood sugar/glucose levels in well term infants without any risk factors.
- BSL/TBG should be measured no more than 2 hours after birth in infants with risk factors for hypoglycaemia.
- If BSL < 2.6 mmol/L at any time, ongoing measurement should be by TBG. 3
Establishing feeding
- Initiate feeds within 30 to 60 minutes of birth.
- Mothers of infants at risk of hypoglycaemia who choose to breastfeed may have been advised to express antenatally and have expressed breast milk available. 15
- Discuss feeding cues with parents and carers.
- Feed at least 3-hourly or more frequently.
- Consider gastric tube feed if infant ≤ 35 weeks.
Infants requiring treatment for hypoglycaemia should be referred to a doctor. Screening blood samples do not need to be taken prior to each feed in infants who are feeding frequently (< 3-hourly) or cluster feeding. They should be taken at 3 to 4-hourly intervals, prior to a feed. Measurement should continue until 3 consecutive BSL/TBGs ≥ 2.6 mmol/L and feeding is assessed as adequate. 16
Prevention of hypoglycaemia in neonatal units
Refer to Management of hypoglycaemia in neonatal units - flow chart 2.
- All preterm infants (< 37 weeks’ gestation) are at risk of hypoglycaemia due to inadequate glycogen stores, inefficient or absent enteral feeding, blunted counter-regulatory responses to low blood glucose concentrations and transient hyperinsulinism resulting from perinatal stress (hypoxia, intrauterine growth restriction, etc.).
- Ensure normothermia.
- Provide an exogenous glucose source within one hour of birth: Consider parental choices.
- breastfeed/ expressed breast milk (EBM)
- formula (with parental consent and if medically appropriate)
- IV glucose (calculate and document IV glucose delivery rate in mg/kg/min using a glucose calculator (e.g. https://nicutools.org/).
Screening
- Measure TBG 1 hour after birth.
- Screening should continue pre-feeds or 3-hourly if infant is nil orally.
- Screening may be performed twice daily if on IV fluids with stable TBG.
- Screening may be discontinued when infant is on full enteral feeds with 3 consecutive TBG’s ≥ 2.6mmol/L without intervention.
Establishing feeding
- Screening should be recommenced if the feeding regimen changes (e.g. transition from EBM/formula to exclusive breast feeds) or if the infant’s clinical condition changes.
- Continue enteral feeds as tolerated and support breastfeeding as per parental choice.
- Increase feeds gradually, reducing IV glucose infusion accordingly when TBG readings are stable (at least 2 consecutive readings ≥ 2.6 mmol/L).
- Infants on three hourly sucking feeds, are otherwise well and of appropriate size and maturity may be transferred to postnatal ward as soon as TBG ≥ 2.6 mmol/L on 2 consecutive occasions. Monitoring should continue on the postnatal ward as per Flowchart. If hypoglycaemia has occurred, complementary feeds after breastfeeding may be necessary for 1 to 2 days until maternal breastmilk supply is established.
Persistent hypoglycaemia
Persistent hypoglycaemia occurs when hypoglycaemia persists beyond 4 hours despite treatment, or where episodes of hypoglycaemia occur ≥ 3 times in 24 hours. 7
Persistent hypoglycaemia may reflect hyperinsulinism, inadequate availability of substrate or increased metabolic demand.
Management comprises of increasing the glucose supply and investigating for severe or prolonged hypoglycaemia.
Infants with hyperinsulinism should continue small enteral feeds where possible. 17
Treatment/medications
Treatment options include the following.
40 % glucose gel
0.5 mL/kg 40% glucose gel is the first-line treatment for hypoglycaemia in well infants ≥ 34 weeks’ gestation. 16 Glucose gel is massaged into the buccal mucosa. It is never for oral administration.
Administration of 40% glucose gel by buccal route:
- Dry the inside of the infant’s cheek with gauze.
- Measure the required amount of glucose gel with oral dispenser.
- Using a clean, gloved finger, apply small amounts of gel at a time to the buccal mucosa (inside the cheek) and massage gently to ensure absorption.
- Do not put the gel in the back of the mouth and make sure that the throat does not become blocked by the gel
- Nurses may initiate 2 doses of glucose gel.
- Doctors may order up to 4 additional doses – maximum 6 doses in the first 48 hours after birth.
IV glucose
Give an IV bolus of 2 mL/kg of 10% glucose followed by a continuous IV infusion of 10% glucose at 60 mL/kg/day to prevent rebound hypoglycaemia.
Increase glucose supply
- Increase frequency of enteral feeds (e.g. 2-hourly), maintain same total volume.
- Increase total fluid intake incrementally by 10 or 20 mL/kg/day to a maximum of 100 mL/kg/day (IV only) or 120 mL/kg/day (enteral as tolerated) within the first 24 hours of life.
- Increase concentration of delivered glucose if hypoglycaemia is persistent:
- 12.5% glucose may be given via a peripheral venous cannula
- 15% glucose MUST be given via central venous line i.e. umbilical venous catheter (UVC) or peripherally inserted central catheter (PICC). May be given via peripheral cannula whilst obtaining central access.
Table 1: Additive calculations to prepare 12.5% and 15% Glucose infusion
| Fluid to be prepared | Fluid bag (500 mL) | Volume to withdraw before additions are made | Additions 50% glucose |
|---|---|---|---|
| Glucose 12.5% | Glucose 10% | Nil | 35 mL |
| Glucose 15% | Glucose 10% | 50 mL | 70 mL |
Adapted from https://pig.rch.org.au.acs.hcn.com.au/appendices/iv-fluid-calc-500ml/18 (login required)
Calculate glucose infusion rates using a glucose calculator (e.g. https://nicutools.org/).
Glucagon
- Glucagon may be used as an intramuscular (IM) injection (200 mcg/kg/dose. Do not exceed 1mg/dose) for the emergency management of hypoglycaemia in infants ≥ 34 weeks’ gestation, or as a continuous infusion (5–20 mcg/kg/hour) where hypoglycaemia is treatment resistant (i.e. infants with hyperinsulinism).
- Allows mobilisation of hepatic glycogen stores.
- Glucagon is less likely to be useful in infants < 34 weeks (due to minimal glycogen stores) or infants > 24 hours postnatal age with inadequate feeding (stores deplete within 24 hours).
- Glucagon IM injection may be repeated once if the initial response was good i.e. TBG ≥ 2.6 mmol/L.
Advice regarding escalation of care
Indication for urgent escalation (e.g. Medical Emergency Team (MET) call):
- TBG < 1.5 mmol/L at any time.
Indications for neonatal unit admission:
- TBG < 1.5 mmol/L at any time.
- TBG < 2.6 mmol/L 2 hours after initiation of treatment.
- TBG < 2.6 mmol/L on ≥ 3 consecutive pre-feed samples.
- Infant appears unwell.
Any infant requiring a glucose infusion rate of > 10 mg/kg/min should be investigated for hyperinsulinism and may require further management.
Advice regarding escalation of care beyond local service
There should be a discussion with Paediatric Infant Perinatal Emergency Retrieval (PIPER) 1300 137 650 if an infant is requiring a Glucose Infusion Rate (GIR) >10mg/kg/min at any time. Calculate the GIR in mg/kg/minute including IV fluids and enteral feeds. www.nicutools.org
Discuss with a paediatrician, retrieval neonatologist, or paediatric endocrinologist.
Any infant with severe hypoglycaemia (glucose infusion rate of > 10 mg/kg/min) or in whom hypoglycaemia presents after 48 hours, or where hypoglycaemia is prolonged (beyond 48–72 hours), or associated with a dysmorphism [exomphalos, ear notching, hemihypertrophy, macrosomia (Beckwith-Wiedemann syndrome), micropenis, ambiguous genitalia, cleft lip/palate, or other midline facial defect, (hypopituitarism, septo-optic dysplasia)] further investigations should be undertaken.
Investigations for severe or prolonged hypoglycaemia
The following investigations may be performed together, or in a tiered way as described below. Of note, if there are concerns that hypoglycaemia may be the result of an inborn error of metabolism, ammonia, lactate and acyl-carnitine samples should be sent urgently regardless of TBG value.
Hypoglycaemia screen
Hypoglycaemia screen 19 to investigate the hormonal response to low blood glucose concentrations, should be performed when TBG < 2.0 mmol/L) and is most useful when done more than 48 hours after birth. 5
Tier 1 investigations: venous or arterial samples – to exclude hyperinsulinism and panhypopituitarism
- Insulin
- Glucose (simultaneously with insulin level)
- Cortisol
- Growth hormone.
- Sodium, potassium
If insulin secretion is not suppressed (i.e. not zero) and the diagnosis of hyperinsulinism is established, continue to treat and in severe cases, with input from the paediatric endocrinologists at the Royal Children’s or Monash Children’s Hospitals and/or PIPER.
If the insulin concentration is suppressed, the diagnosis of hyperinsulinism is not established then tier 2 investigations should be performed.
Any abnormal growth hormone or cortisol levels requires tier 2 investigations.
Tier 2 investigations: to exclude panhypopituitarism and congenital adrenal hyperplasia
- 17-hydroxyprogesterone (17-OHP)
- Thyroid function (TSH and FT4)
- Urine osmolality and specific gravity
- Cranial ultrasound
- Eye examination by ophthalmologist
- Growth hormone and cortisol (if not already done with tier 1 investigations)
Tier 3 investigations: to exclude inborn errors of metabolism (RCH metabolic guideline)
If hypoglycaemia persists despite normal tier 1 and tier 2 investigations, or where there are clinical features consistent with metabolic disease (encephalopathy, cardiomyopathy), the following tests should be performed without delay and advice sought from the RCH metabolic team:
- ammonia level (free flowing sample)
- lactate and pyruvate (arterial sample)
- free fatty acids and acyl carnitine profile
- triglyceride level
- urine organic acids
- urine metabolic screen, including reducing substances and ketones
- plasma amino acids
- accelerated completion of the newborn screening test - contact the Victorian Clinical Genetics Services screening laboratory and ask for the infant to be flagged as having a possible metabolic disorder.
Follow-up
Infants managed for hypoglycaemia in the postnatal ward do not require routine outpatient follow-up.
Infants admitted to a neonatal unit for management whose hypoglycaemia is refractory to simple intravenous therapy should be reviewed post discharge according to specialist endocrine advice.
Management flow charts
To be used in conjunction with this guidance:
- Flow Chart: Management of hypoglycaemia in birthing environments and postnatal wards
- Flow Chart: Management of hypoglycaemia in neonatal units
References
- Harris DL, Weston PJ, Gamble GD, Harding JE. Glucose profiles in healthy term infants in the first 5 days: the glucose in well babies (GLOW) study. J Pediatr (2020) 223:34–41. 10.1016/j.jpeds.2020.02.079
- Kaiser JR, Bai S, Gibson N, Holland G, Lin TM, Swearingen CJ, Mehl JK, ElHassan NO. Association between transient newborn hypoglycemia and fourth-grade achievement test proficiency: a population-based study. JAMA Pediatrics. 2015 Oct 1;169(10):913-21.
- McKinlay CJ, Alsweiler JM, Anstice NS, Burakevych N, Chakraborty A, Chase JG, Gamble GD, Harris DL, Jacobs RJ, Jiang Y, Paudel N. Association of neonatal glycemia with neurodevelopmental outcomes at 4.5 years. JAMA Pediatrics. 2017 Oct 1;171(10):972-83.
- Kaiser JR, Bai S, Rozance PJ. Newborn plasma glucose concentration nadirs by gestational-age group. Neonatology. 2018;113(4):353-9.
- McKinlay CJ, Alsweiler JM, Ansell JM, Anstice NS, Chase JG, Gamble GD, Harris DL, Jacobs RJ, Jiang Y, Paudel N, Signal M. Neonatal glycemia and neurodevelopmental outcomes at 2 years. New England Journal of Medicine. 2015 Oct 15;373(16):1507-18.
- Glasgow MJ, Harding JE, Edlin R, CHYLD Study Team. Cost analysis of cot-side screening methods for neonatal hypoglycaemia. Neonatology. 2018;114(2):155-62.
- Jane E Harding, Jane M Alsweiler, Taygen E Edwards, Chris JD McKinlay. Neonatal Hypoglycemia. BMJ Med. 2024; 3(1): e000544. Published online 2024 Apr 9. doi: 10.1136/bmjmed-2023-000544
- The Women’s Hospital Clinical Guidelines: Hypoglycaemia – Newborn management. Updated July 2024. Available from: https://www.thewomens.org.au/health-professionals/clinical-resources/clinical-guidelines-gps. [reviewed July 2024; Accessed August 2024]
- World Health Organization: The WHO Child Growth Standards http://www.who.int/childgrowth/standards/en/a [Accessed August 2024]
- www.ucalgary.ca/fenton accessed [August 2024]
- https://intergrowth21.com/tools-resources/newborn-size [accessed August 2024]
- Farmey A Joseph, Jonathan A Hyett, Philip J Schluter, Andrew McLennan, Adrienne Gordon, Georgina M Chambers, Lisa Hilder, Stephanie KY Choi and Bradley Vries. New Australian Birthweight Centiles. Med J Aust 2020; 213 (2): 79-85. || doi: 10.5694/mja2.50676
- Queensland Clinical Guidelines. Hypoglycaemia-newborn. 2023; Available from: http://www.health.qld.gov.au/qcq [Accessed August 2024]
- Harris DL, Weston PJ, Harding JE. Incidence of neonatal hypoglycaemia in babies identified as at risk. The Journal of Pediatrics. 2012 Nov 1;161(5):787-91.
- Forster DA, Moorhead AM, Jacobs SE, Davis PG, Walker SP, McEgan KM, Opie GF, Donath SM, Gold L, McNamara C, Aylward A. Advising women with diabetes in pregnancy to express breastmilk in late pregnancy (Diabetes and Antenatal Milk Expressing [DAME]): a multicentre, unblinded, randomised controlled trial. The Lancet. 2017 Jun 3;389(10085):2204-13.
- Harris DL, Weston PJ, Signal M, Chase JG, Harding JE. Dextrose gel for neonatal hypoglycaemia (the Sugar Babies Study): a randomised, double-blind, placebo-controlled trial. The Lancet. 2013 Dec 21;382(9910):2077-83.
- Tottman AC, Bloomfield FH, Cormack BE, Harding JE, Slim MA, Weston AF, Alsweiler JM. Relationships between early nutrition and blood glucose concentrations in very preterm infants. Journal of Pediatric Gastroenterology and Nutrition. 2018 Jun 1;66(6):960-6.
- The Royal Children’s Hospital Paediatric Injectable Guidelines-Online by subscription. Updated 2024. [Accessed August 2024] https://pig.rch.org.au/
- Thornton PS, Stanley CA, De Leon DD, Harris D, Haymond MW, Hussain K, Levitsky LL, Murad MH, Rozance PJ, Simmons RA, Sperling MA. Recommendations from the Pediatric Endocrine Society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. The Journal of pediatrics. 2015 Aug 1;167(2):238-45.
Citation
To cite this document use: Safer Care Victoria. Hypoglycaemia in Neonates [Internet]. Victoria: Neonatal eHandbook; 2024 [cited xxxx] Available from: https://www.safercare.vic.gov.au/clinical-guidance/neonatal
Flowchart 1: Management of hypoglycaemia in birthing or postnatal ward
Flowchart 2: Management of hypoglycaemia in the neonatal unit
Downloads
Get in touch
Version history
First published: February 2018
Reviewed: October 2024