Find out what the stages are in a typical surgical journey – from when you first find out you may need surgery to going home after your surgery.
If you would like an interpreter, you can access one here.
Do I need surgery
View more View lessSurgery is not right for everyone. It is important you talk to your healthcare team about your treatment options and decide together about your treatment plan.
What other options do I have?
There may be other options you can try instead of surgery. These are called alternative therapies or non-surgical treatments. Some examples of alternative therapies include:
- orthopaedic clinics
- hand therapy clinics
- physiotherapy
- occupational therapy
Your healthcare team can provide you with more information and discuss what options are right for your situation.
What is shared decision making?
Shared decision making is when you discuss your health and treatment options with your healthcare team and decide on a treatment plan together. This process allows you to ask questions and weigh up your options so that you can make a decision you are happy with.
It involves talking with your healthcare team about your values, goals and preferences for your care. You and your healthcare team consider these alongside evidence about the benefits and risks of treatment.
Tools to help me with shared decision making
To learn more, see Choosing Wisely Australia’s resource – Five questions to ask your doctor or other healthcare provider before you get any test, treatment, or procedure.
Sharing my health history with my healthcare team
It’s important that you share your health history with your team. Your team need to know about your health conditions and medications. This helps the team identify possible surgery risks, the right treatment options and organise tests before your surgery.
It’s helpful for you to tell your healthcare team about:
- allergies
- airway difficulties, obstructive sleep apnoea, or if you snore or wake up gasping for air
- medications, in particular blood thinners and medications that reduce your ability to fight infection
- anything else you think they should know.
What if my condition changes?
It’s important to let your healthcare team know if your health:
- gets better, for example, you have completed some physiotherapy and you feel stronger, your symptoms improve, or
- gets worse, for example, you are walking less, or your other health conditions are not controlled.
Meeting my healthcare team
Throughout your surgical journey, you will work closely with your healthcare team – they are there to support you. See Meeting my healthcare team for a list of who your potential healthcare team may be.
I've decided to have surgery
View more View lessGetting ready for surgery and my recovery
Staying active and eating well in the months before your surgery will help your recovery.
Book a GP appointment in the months before your surgery if you have other health conditions that need management.
Speak to your healthcare team about your surgery options, if you are:
- over 65 years old
- not very active
- needing help with daily tasks
- losing your balance easily or have fallen over before
- having difficulty with memory and thinking.
Once you’ve decided to have surgery you will be asked to give your informed consent. You can refuse or withdraw your consent at any time before the surgery.
See the printable 'Getting ready for surgery and my recovery checklist' under 'Resources' to help you prepare for your surgery.
What I can do to boost my health before surgery
There are key things you can do to boost your health before surgery with the guidance of your healthcare team.
Here is a list of what you can do to help have a faster recovery:
- Exercise – staying active before your surgery is important and can help you get stronger so your body can repair quickly.
- Diet and nutrition – getting the right nutrition assists with:
- fast wound healing
- optimising and maintaining your weight
- building and maintaining your strength.
- Mental health/emotional wellbeing – mentally preparing for surgery is as important as preparing physically. The leadup to surgery can be stressful. Some things you can do to help manage this are talking to your support person, regular exercise and speaking with your healthcare team.
- Alcohol intake – it is advised not to drink alcohol, or limit your alcohol intake, in the months before your surgery.
- Smoking, vaping, and illicit drugs – avoiding smoking, vaping and the use of illicit drugs in the months leading up to your surgery. If this is difficult for you, speak with your healthcare team. For more information, see the Quit website.
- Sleep – have a regular sleep pattern leading up to your surgery and try to maintain this pattern during your recovery.
- Intimacy – the type of surgery you have may impact on relationship intimacy. To get information that is relevant to you, discuss this with your healthcare provider.
Ask your healthcare team for more information.
What I need help with
Reviewing my medical conditions
Meeting with your local doctor (GP) to review your medical conditions is recommended as they can impact on surgical outcomes. It can take time to optimise medical conditions, so it is helpful to make a GP appointment well in advance of your surgery.
Some examples of the things your local doctor may review are:
- Medications –Stopping or pausing medications can pose a risk and it is important this is monitored closely with your healthcare team.
- Mental health
- Medical conditions –Some of the more common conditions you should talk to your healthcare team about are:
- anaemia (lack of healthy red blood cells)
- heart disease
- arterial fibrillation (abnormal heart rhythm)
- diabetes
- high or low blood pressure.
Tests before my surgery
Before your surgery, your healthcare team might request some tests.
If you are having difficulty getting these tests done, make sure you discuss it with your health care team.
Preparing ahead for my discharge home
Before having surgery, it’s important to prepare for your recovery and discharge home.
Some examples of planning ahead might be:
- arranging someone to look after your pets while you’re in hospital
- having someone stay with you when you get home.
How many days will I be in hospital?
Your healthcare team will discuss with you how long you need to stay in hospital.
Many factors impact how long you stay in hospital. These factors can be:
- medications you are on
- your level of physical activity before the surgery
- your supports at home
- other health conditions you might have.
For more information about surgery options, see Day surgery on Better Health Channel.
What to expect for my recovery in hospital
Everybody will recover from surgery differently. Things like age, prior levels of physical activity and the type of surgery you have can affect your recovery.
On the day of your surgery, your physiotherapist or nurse will get you out of bed standing and walking as soon as it is safe. This may feel like it is quick to get moving but evidence shows the faster you get moving, the faster your recovery.
How will I get home from hospital?
Before coming into hospital for surgery it’s important to arrange for someone to drive you home once you’re discharged. It’s often recommended not to drive for at least 24 hours after surgery.
Speak with your healthcare team to understand how long you can’t drive for as you will need to plan for this.
If you don’t have anyone available to drive you, speak with your healthcare team early to help you arrange a safe way to get home.
Preparing ahead for my recovery at home
Learn about signs and symptoms
Ask your healthcare team for a list of what signs and symptoms you should be looking out for after your surgery and show this list to your support person.
Equipment needs
Equipment may be needed during your recovery to help you walk, dress, use the bathroom, shower or relieve pressure from a wound.
It is also important for your recovery to follow your walking recommendations, such as using walking aids, crutches or walking frame.
If you have a disability or require additional support when you get home, make sure to tell your healthcare team early so it can be arranged before you get home.
Support from community services or family and friends after surgery
Your healthcare team may arrange short-term community services if you need extra help. This may include help for:
- personal care (for example, showering)
- home care (for example, shopping and cleaning)
- community nursing or allied health (for example, physiotherapy).
Sometimes it can feel overwhelming to navigate community care and to know what you need. If you need help, a social worker, liaison officer or similar team member will be able to assist you and your family.
If you have day surgery, you will require a support person or carer to monitor you and care for you on your first night. If you don’t have a support person to stay with you, talk to your healthcare team about options.
Support for your carer
As a carer if you are concerned about the patient, speak with the healthcare team. See Carers resources, in Resources.
For more information about support for carers, see Carer services and support on Better Health Channel.
What are my discharge options?
Talk with your healthcare team about the discharge options your hospital provides and what will be safe for you.
Recovery and rehabilitation can take place either in hospital or at home.
I've been given my surgery date
View more View lessIf you have questions or concerns about your surgery date or your circumstances change, please speak with your healthcare team as soon as possible.
Book an extended General Practitioner (GP) appointment for after your surgery
When you get a surgery date it’s important to ask your healthcare team if you will need a GP appointment after you get out of hospital. If you do, book an extended appointment time for the week you will be back home.
How will I get to hospital?
Ask your hospital about car parking and pick-up zones so you and your support person know ahead of time where to go.
If you are having difficulty arranging transport speak with your healthcare team.
Week before surgery
Pausing medications
You may need to stop some medications leading up to your surgery, for example, blood thinners. It is essential you understand what these medications might be and that this is discussed with your healthcare team. You can use the printable medications resource to record this information.
What to bring?
To help you prepare, see 'Getting ready for surgery and my recovery checklist' under 'Resources' for advice what to bring to hospital and what to leave at home.
If you are feeling unwell in the 3 days before your surgery, it is very important you tell your hospital if you have:
- a temperature or fever (feeling hot or cold)
- a sore throat, cough or other breathing problems
- a rash or swelling
- been feeling generally unwell
- a cut, break or tear in your skin
- diarrhoea or vomiting
- had a recent unplanned visit to an emergency department or local doctor/general practitioner (GP).
Make sure you know the hospital phone number in advance, so you are prepared if this occurs.
24 to 48 hours before surgery
Fasting
Fasting means stopping eating and drinking before your surgery. Fasting is important when having a general anaesthetic as it keeps you safe during your surgery.
Your healthcare team will provide you with clear instructions explaining when to stop eating and drinking.
The time you start fasting can differ depending on your time of surgery. If fasting is done incorrectly, it can delay your surgery as it increases your risk of complications. Talk to your healthcare team if you are unsure about anything.
You can write your fasting instructions on the 'I've been given my surgery date checklist', see under 'Resources'.
Surgery cancellation
View more View lessHere are the common reasons for surgery to be cancelled.
Hospital has cancelled my surgery
Common reasons include:
- an emergency surgery has taken priority over your scheduled surgery
- lack of beds in the hospital
- the surgeon is no longer available.
The hospital will call and explain if your surgery is cancelled.
My circumstances have changed
If you feel unwell in the days before your surgery, or on the day of surgery, call the hospital or your surgeon to let them know.
Contact your hospital as soon as possible if you:
- change any contact details, such as your address or phone number
- are unable to attend due to work or family commitments
- become pregnant – see Better Health Channel’s Pregnancy page
- have a new medical problem or medication- see Better Health Channel’s Managing treatments and medications
- no longer have a support person or carer to stay with you after surgery
- have concerns about your surgery.
Fasting incorrectly
Surgery can be cancelled if fasting procedures are not followed correctly.
Make sure you understand when you need to stop eating and drinking and what you can eat and drink leading up to your surgery (24-48 hours before).
Medications
Surgery can be cancelled if medications such as blood thinners are not stopped at the right time before your surgery.
It is important to ask your healthcare team when you might need to stop medications and record this on the printable medication records resource.
Day of my surgery
View more View lessIt is common to feel nervous on the day of surgery. This page will walk you through what to expect, from when you arrive at hospital until after your surgery.
Arriving at the hospital
When you get to the hospital you will go to the admissions desk and complete some paperwork.
Once this is successfully completed, they will admit you to hospital.
Admitted by a nurse
The next stage of being admitted to hospital is usually seeing a nurse.
They will ask you some questions about how you are feeling and when you last had something to eat and drink.
They will take some measurements such as:
- blood pressure
- temperature
- weight.
This is also a good time to ask your healthcare team any questions you may have.
Getting changed for surgery
Once you have been admitted by the nurse they will give you a hospital gown, underwear and a hat to wear while you have surgery.
Your belongings will be given to the healthcare team while you are in surgery.
Surgical team review
Just before your surgery you may be seen by your surgeon.
They will discuss your plan for surgery and confirm consent to undertake your surgery.
Anaesthetist review
Around the time you see your surgical team you will also see your anaesthetist.
They will ask your name, date you were born, allergies and what surgery you are having.
A needle may be put into your arm, to give you medication during your surgery.
If you have any questions for the anaesthetist, you can ask them during this review.
Going to theatre
After you have been reviewed by the healthcare team, you will be moved into the theatre. You may be lying on a bed, trolley or you might walk into the.
Don’t be alarmed if there are lots of people in the theatre, they are there to help the surgeon. There may also be bright lights and equipment the surgeon needs to perform the surgery.

Getting an anaesthetic
Your anaesthetist will give you medication to sedate you (make you feel sleepy) and/or numb the area of your surgery (nerve block).
They will stay with you throughout your surgery to make sure you are safe.
Recovery area
Once your surgery has finished, specialised nurses will monitor you as you start to wake up from your surgery in the recovery area.

Going to a hospital ward or being discharged home
Once the healthcare team are happy you have recovered from the anaesthetic, you will move out of recovery.
If you need more time in hospital, you will move to an inpatient ward. Your healthcare team will get you out of bed and moving so you can get home quickly.
If you are having day surgery, your support person will pick you up and take you home. It is recommended not to drive for at least 24 hours after surgery.
After my surgery
View more View lessMy recovery in hospital
On the day of, or day after surgery, your healthcare team might encourage you to complete some tasks to help you recover faster. These tasks may include:
- standing and walking as soon as it is safe (early mobilisation)
- sitting out of bed and upright for all meals
- deep breathing and coughing exercises
- showering and dressing in your own clothes
- eating and drinking
- monitoring how frequently you are going to the toilet
- providing you with exercises to complete.
Monitoring your recovery
During your stay in hospital, you will have your blood pressure, oxygen saturation level (amount of oxygen in your blood), temperature, heart rate and pain monitored. These are called your vital signs.
The healthcare team will check your wound and ask if you have opened your bladder or bowels (done a wee or poo). They may also ask about your thinking and memory. These are key factors that may impact your discharge home.
Eating and drinking
Soon after your surgery you will be able to eat and drink (unless your healthcare team have advised against this).
Pain
Pain can happen after surgery. The type of surgery you have, as well as your preparation before surgery, can impact your pain levels. Your healthcare team are there to help manage any pain you may be feeling and are experienced in making you as comfortable as possible.
It is important to discuss your pain levels with your healthcare team to work out the best way to manage your pain in hospital and once you are home.
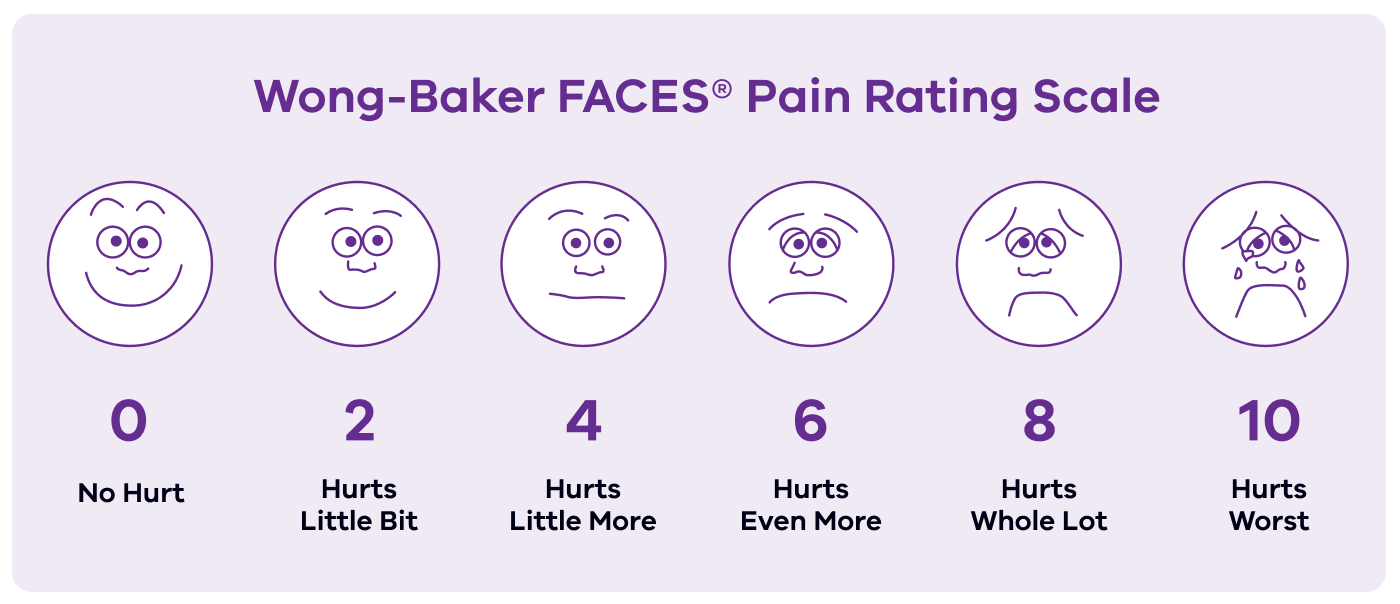
You may be asked to rate your pain levels on a scale of one to 10. The following diagram is an example of what you may be shown to help with this process.
Medications after surgery
Speak with your healthcare team while in hospital to understand if you have new medications and if you will need them once you go home. For example, anti-coagulants (medication that helps thin your blood) might be needed after some surgeries. You may start this medication in hospital and may need to continue taking this medication temporarily once you’ve been discharged home.
I’m feeling unwell
When you are in hospital you or your carer may have concerns that you aren’t feeling well or are feeling worse after your surgery. If you notice changes in yourself, or your loved one’s health, it is important you speak with your healthcare team.
Some hospitals may have a program or people such as patient liaison officers (PLO) that you can speak with. Contact them if you have raised your concerns with your healthcare team and you are still feeling concerned.
I’m ready to go home
Before you leave hospital there are some things your healthcare team will check with you. These things might be:
- making sure you have been to the toilet (bladder and bowels)
- looking at the distance you can walk and if you can use stairs. This is to check you can walk around your home and get in and out safely
- making sure have the equipment you need for home
- removing any catheters or needles unless you need them at home
- you will be given a discharge plan that outlines your surgery and recovery.
Use the 'I'm ready to go home checklist' to make sure you are ready to leave hospital, see under 'Resources'.
Medications after surgery
Before leaving hospital, a member of your healthcare team, for example a pharmacist or nurse, will discuss your medication plan. This plan outlines your regular medications and new medications. It should guide you on when to stop, start and restart medications.
You may start new medications in hospital and may need to continue taking this medication temporarily once you’re discharged home. The hospital may provide you with a small supply of new medications or a script for you to get the medication from a community pharmacy.
Before any new medication runs out, you will need to see your GP to discuss your ongoing medication plan after surgery.
Note: Some medications can interact with alcohol and other drugs so ask your healthcare team about this before you leave hospital. Some examples are medications for pain or infection (antibiotics).
Wound care
Once you are ready to go home, your healthcare team will provide you with information on how to manage the wound.
It is also important to understand signs of infection and who to contact if you are worried about your wound.
Services and support
After surgery, some people may need short-term services and support (for example, community nursing, personal care and home care) after a hospital stay.
If you had existing services before your surgery, then you may need to speak to the provider to reinstate these. Speak to your healthcare team to check that the services you had before your surgery are enough to support your early recovery at home.
Date and time for follow-up appointments
Before you leave hospital ask your healthcare team what appointments you may need.
If an appointment time isn’t booked before you leave hospital, ask how you will be notified of the appointment date and time.
What if I need help when I get home?
Before you leave hospital, it is helpful to understand what signs or symptoms after surgery can indicate you need to seek help. Ask your healthcare team what you should be looking out for.
When you leave hospital ask your healthcare team if there is a contact number for you to call if something goes wrong at home.
If you are unsure what to do or who to call about your signs and symptoms, you can contact:
- your local doctor/GP – if you don’t have one you can use the HealthDirect Service finder
- your local Priority Primary Care Centre
- NURSE-ON-CALL for assistance and advice from a registered nurse 24 hours a day- call 1300 60 60 24
- Victorian Virtual Emergency Department, a public health service to treat non-life-threatening emergencies - visit vved.org.au
- If you think your situation is an emergency, you should always call Triple Zero (000) or go to an emergency department.



